We see the numbers a lot: estradiol, estrogens, FSH. But what do they mean, and what can they actually tell a woman about where she is in the menopause transition?
Turns out, the team at Gennev found that using a menopause hormone levels chart may be less helpful than we’d like.
While there are uses for having hormone levels tested, pinpointing your place on the perimenopause-to-menopause journey probably isn’t one of them. Hormones just don’t cooperate during this time (which is probably why you’re wanting to get them tested in the first place), and hormone tests can only really offer a limited snapshot of where you are right now as which is probably not where you’ll be tomorrow.
To understand all this better, we had a Q & A with our ob/gyn Chief Medical Officer, Dr. Rebecca Dunsmoor-Su, on to test or not to test.
What is the reason for testing hormone levels?
Dr. Rebecca: Good question. Hormone levels are helpful when we are tracking fertility and ovulation induction [using hormonal therapy to prompt an ovary to release an egg]. Taken several times, they can give a very tentative window into where in the fertility transition a woman is.
But as and this is a big but as hormone levels are extremely variable throughout the cycle and even more irregular during the perimenopausal transition, so they become much less useful.
Looking At A Menopause Hormone Levels Chart
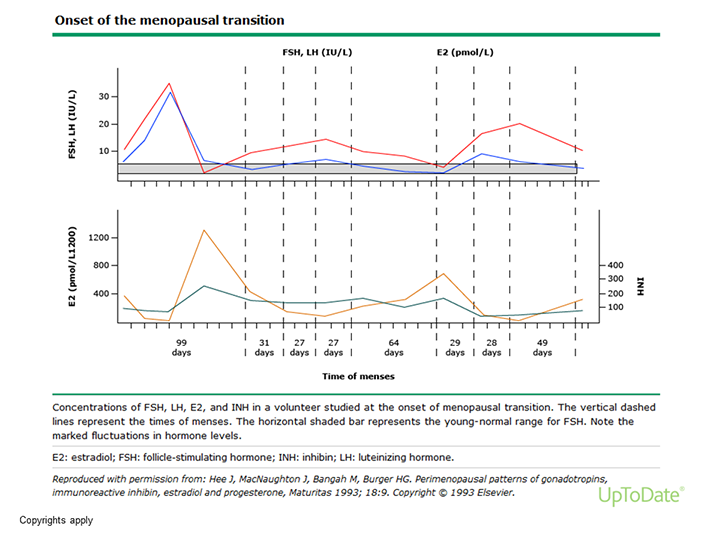
This graph is of hormone levels in one woman over the course of 1 year in perimenopause. At the bottom you can see the spacing between her periods, which is very irregular. During this year her cycles vary from 99 to 20 days long. In the top graph are measurements of her FSH and LH, but if you look at how varied the FSH is (solid line), you’ll notice that there are several time points where if measured it looks “normal” and several where it looks “post-menopausal” and lots in the middle. This is why it is not reliable. In the bottom chart you can see that her estrogen measurements are similarly irregular and all over the place (the dotted line) but most of the time are within the “normal” range.
Is it ever useful to check hormone levels for women in perimenopause or menopause?
Dr. Rebecca: In my experience, I almost never check them. If a woman has a uterus, than where she is in menopause or perimenopause is best determined by her cycles, or lack thereof.
If a woman has had a hysterectomy, we go by symptoms. We may check FSH [follicle-stimulating hormone] if these are unclear, but again, because it can be so variable, it may not tell us much.
Fundamentally it feels important to know where you are “in menopause,” but really we need to know if you are symptomatic, and we will treat that. Menopause is a normal and natural transition for women that requires no medication if a woman is not having problematic symptoms. If your symptoms are problematic, then we should treat you, no matter where you are in that transition.
What are these tests testing for?
Dr. Rebecca: If correctly done, they look at the relative levels of FSH, progesterone, and LH (leutenizing hormone) to try to get a window into the hormones at a certain point in a woman’s cycle. They are best understood at the “day 3” point of the cycle, i.e. the 3rd day after the start of your period. This is when we have the most data about what they should look like. Random values of these hormones are not helpful.
What do the numbers mean?
A woman reported her numbers as “Estrodial: 8.2, Estrone: 23.3, Total Estrogens: 31.5″ as what does that tell her or her doc?
Dr. Rebecca: Not much at all. What day of her cycle is she on? What is her FSH? When did she last have a period? What medications is she taking? I can’t interpret these tests without all that information.
Additionally, while there is a range of m=normal estradiol levels for women, they vary over the cycle, and between women. If the patient has symptoms, we should be treating her; if she doesn’t, then there is no need to treat, no matter what the values are. Also, just estradiol is needed, that is the active hormone; testing the rest doesn’t add any information (though it does add cost…). There are much better menopause tests for diagnosis available.
Why do doctors conduct these tests if they’re not truly useful?
Dr. Rebecca: Some physicians do not understand the cycle well and think that these tests help. A lot of these tests can help us talk about fertility, and if a physician is not menopause savvy they may not understand the difference in usefulness.
Some providers are getting some money from the tests in “special labs.” Some use them to prescribe expensive hormones or supplements that are no better than the pharmaceutical ones as in fact, they are probably less safe.
A big red flag I need to point out: if your provider tells you “only they understand” how this works, or only they have the answer and the rest of the medical community is “behind” or “ignorant” or “just doesn’t understand” and only they can sell the exact product you need, run away.
Any well-trained menopause provider should truly understand how hormones work and change in the perimenopause. We all have access to charts like the perimenopausal transition chart and the STRAW staging of menopause, and we can tell by symptoms and periods about where you are. We all know how to prescribe HRT properly and will recommend that you use an FDA-regulated product.
Compounded hormones are no more “bio-identical,” in fact they are generally a pharmaceutical product which is crushed and compounded into a cream. So it’s the same medication I would prescribe, now less reliably absorbed and dosed.
What are better indicators of where women are in the menopause transition?
The menopause is defined based on menstrual cycle. The most common pattern is that first cycles become just a little shorter (21-25 days instead of 28-32). Then they start to space out, and women will occasionally skip periods (see the perimenopausal transition chart).
During this time, some months the ovaries are working normally, some they are behind, but eventually they’ll recruit an egg. Sometimes they just don’t make it to an ovulation, and the lining of the uterus sheds in a irregular fashion because it got too thick (this is usually a long, heavy period bleed).
During this whole time period, hot flashes and night sweats can be present. Eventually, periods will stop, and after there have been no menses for one year, you are menopausal.
Is there some way to know (or approximate) when symptoms will begin to lessen and finally end?
Symptoms are very individual. In general, hot flashes and night sweats can start 1-3 years before the last period and last on average between 2-6 years. Some women experience them up to 10 years. Vaginal dryness and vaginal issue symptoms happen in about 50 percent of women, and generally don’t start to be a problem until 1-2 years after the last period. Cardiovascular risks and cholesterol changes, bone changes all start when the periods stop.
Can women use this information to make decisions like whether to begin HRT?
HRT is generally prescribed for symptoms, and so we would treat based on that. We no longer generally prescribe systemic HRT for bones or heart health (though it can be helpful for those things too).
HRT is not a “fountain of youth,” though there is some evidence that women who use HRT may live longer. However, the studies were not designed to look at that, so we can’t be sure that this isn’t because they weren’t healthier to begin with.
Knowledge is power as and so many women feel powerless during this time. What tools do we have to empower women for real?
Gennev is a wonderful and empowering resource. A NAMS-certified menopause practitioner is also a great resource. Ask your OB/GYN if they are comfortable with menopause care and hormones.

It would be nice to put an end date on menopausal symptoms, but hormone-level testing probably won’t get you any closer to an answer than a discussion with your doctor will.
If you’re ready to better understand where you are in the perimenopause > menopause transition, take Gennev’s Menopause Assessment. You may be surprised to discover some of the issues you’re having are actually related to hormones. Then, take your results to your doctor as or consult with one of our menopause specialists via Gennev’s telehealth.
We can help you understand where you are in your menopause journey
- Meet with a Gennev board-certified gynecologist who is a menopause specialist – they can give you a trusted opinion, determine if medication is right for you, and provide prescription support.
- Try Vitality as our nutrient-packed multi-vitamin supplement supports your whole body including mood, energy, stress response, immune health, joint pain, and inflammation. 96% of women report having more energy after just 2-weeks with Vitality.
The information on the Gennev site is never meant to replace the care of a qualified medical professional. Hormonal shifts throughout menopause can prompt a lot of changes in your body, and simply assuming something is “just menopause” can leave you vulnerable to other possible causes. Always consult with your physician or schedule an appointment with one of Gennev’s telemedicine doctors before beginning any new treatment or therapy.
